Assessing the Process of Written Informed Consent for Surgical Procedures among Inpatients: A Cross-sectional Study from a Tertiary Care Teaching Hospital in Southern India
V. Dinesh, Imaad Mohammed Ismail, Kahkashan Azeez
Journal of Clinical & Diagnostic Research, 2024
Abstract
Introduction
Informed Consent (IC) is a decision-making process wherein patients are provided with all necessary information regarding treatment to make an uncoerced, educated choice. There are gaps in the implementation of the IC process that need to be identified and addressed.
Aim
To estimate the proportion of patients/surrogates who read, understood, and signed the IC form before undergoing surgical procedures; to identify the different healthcare team members involved in explaining the IC form; to evaluate the extent to which different components of the IC form were explained to patients/surrogates; and to determine the influence of the IC form on surgical decision-making, and the overall satisfaction with the IC process.
Materials and Methods
This cross-sectional study was conducted at a tertiary care hospital in the Dakshina Kannada District of Southern India from April 2020 to March 2021. It included 100 adult patients admitted to the postsurgical wards of general surgery, orthopaedics, obstetrics and gynaecology, otorhinolaryngology, and ophthalmology. Ethical clearance was obtained from the Institutional Ethics Committee. The parameters studied included socio-demographic variables, administration of the IC form, details on the person explaining the IC form along with its content, and the influence of the IC form on decision making, as well as overall satisfaction with the IC process. Data were collected using a predesigned questionnaire and analysed using descriptive statistics in Statistical Package for the Social Sciences (SPSS) version 27.0. Categorical variables were presented as frequencies and proportions, whereas continuous variables were presented as means and standard deviations.
Results
All participants received the IC form; however, only 21% read, understood, and signed it. The explanation of the IC form was given to 59% of the patients, with only 15% of these explanations provided by the treating surgeon. The components of the IC form, such as the surgical procedure and its benefits, were explained to the majority of the patients; however, the risks of the surgical procedure and alternative options were explained to only 53% and 7% of patients, respectively. The IC form had a minor influence on surgical decision-making for 61% of patients, and 43% expressed satisfaction with the IC process.
Conclusion
The study revealed that the implementation of IC was inadequate. Surgeons should provide and explain the IC form well in advance, allowing time for patients to read, understand, and clarify their doubts. Hospital Ethics Committees need to enforce strict adherence to IC guidelines to ensure informed decision-making.
Category: Cultural/Country Context
Consent for organ donation: a case study in the light of bioethics
Consent for organ donation: a case study in the light of bioethics
Health Sciences
Kelly C.B. Gomes, Mary R.G. Esperandio, José E. De Siqueira, José R. Goldim
The Annals of the Brazilian Academy of Sciences, 2024
Abstract
Fewer donations are being made in Brazil to meet the growing organ demand. Organ donation in Brazil reached an average of 53% consent. However, hospitals in Paraná have reached a level of 94.2%. What reasons could be given for these levels? Accordingly, this study aimed to understand the causes involved in decision-making to donate organs. The methodology used was qualitative based on a case study. Data was collected at a hospital in Toledo, a city in Paraná, through documentary research and semi-structured interviews with two distinct groups: professionals responsible for the family approach to donation and five families consenting to donation. The search for data was restricted to the period between 2015 and 2023. Data analysis used Bardin’s content analysis. The results were organized into four categories in the first group, and two categories in the second group, suggesting that aspects linked to bioethical references present in the interview, such as beneficence and autonomy, contribute to the emergence of high rates of family consent for organ donation in the hospital studied. It is recommended for future research to test successful interview models to reverse the current organ donation rates in Brazil.
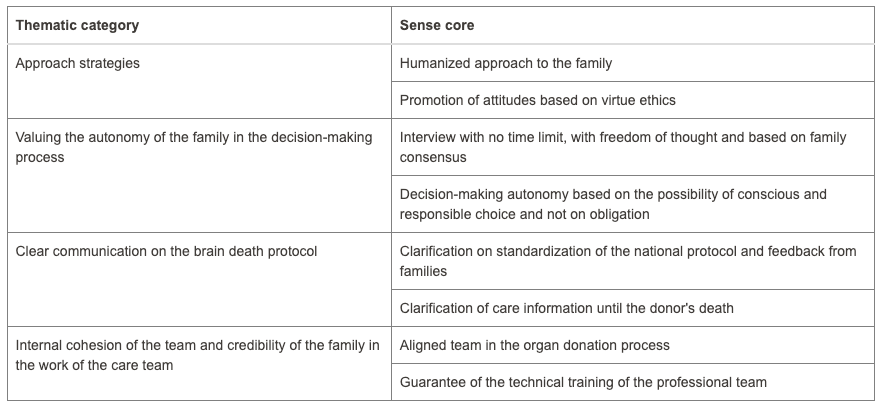
Four categories from the first group as mentioned in the abstract
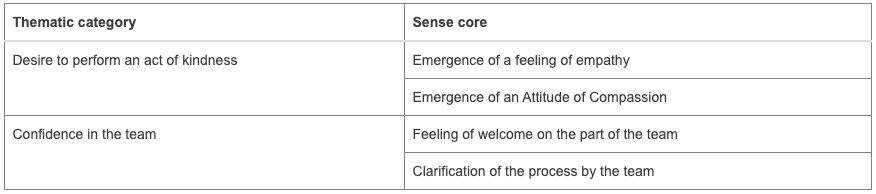
Two categories from the second group as mentioned in the abstract
Analysis of Attitudes Towards Opt-Out Organ Donation Consent: A Cross-Sectional Study Among Saudi Arabian Residents
Analysis of Attitudes Towards Opt-Out Organ Donation Consent: A Cross-Sectional Study Among Saudi Arabian Residents
Sami Alobaidi
Transplantation Proceedings, 24 October 2024
Abstract
Objective
The study aims to investigate public opinion on opt-out organ donation registration in Saudi Arabia, addressing a gap identified in existing research that reveals varied attitudes and intentions among the population, as indicated by studies in Qatar and Saudi Arabia.
Methods
This study employed a secondary analysis approach, utilizing data from a cross-sectional survey conducted online among 1397 residents of Saudi Arabia. The survey utilized a GoogleTM form questionnaire adapted from a previous study in Qatar. The questionnaire comprised three sections, gathering socio-demographic information, assessing general awareness about organ donation, and exploring participants’ agreement with opt-out consent and beliefs related to organ donation using the Theory of Planned Behaviour (TPB) model.
Results
Among the participants, 44.4% supported opt-out consent, with 25.7% females and 39.1% Saudi citizens. Females and diploma/graduation-level education were significantly associated with opt-out support (P < .001, P = .012, respectively). 98.06% of opt-out supporters were familiar with organ donation. 93.05% agreed to promote organ donation, 98.38% believed registration saves lives, and 81.91% were willing if family had no objections. 86.75% were ready with more information, and 85.78% if informed about their religion’s perspective. 92.25% believed living and posthumous donation positively impact life after death. Concerns included inadequate care (33.44%) and bodily disfigurement (28.43%) postmortem. Majority felt healthy (45.56%) and appropriate in age for donation (57.67%). Among opt-out supporters, 20.84% expressed interest, 8.4% conveyed disinterest, while 36.34% remained undecided regarding organ donation registration.
Conclusion
The study reveals a considerable openness among Saudis toward adopting an opt-out organ donation system, suggesting a potential avenue for increased organ donation rates. While acknowledging cultural nuances, particularly familial influences, targeted interventions are vital to overcome specific barriers and ensure the successful implementation of an opt-out policy.
Implementation of Respect for Autonomy in Hospital Services Within the Indonesia National Health Insurance System
Implementation of Respect for Autonomy in Hospital Services Within the Indonesia National Health Insurance System
Desdiani Desdiani, Sri Mulatsih, Diah Ayu Puspandari
National Journey of Community Medicine, 1 October 2024
Abstract
The principle of patient autonomy forms the foundation of medical ethics. However, its exploration within the context of national health insurance systems in developing countries remains under-researched. This study aimed to evaluate respect for patient autonomy within Indonesia’s National Health Insurance (NHI/JKN) system. The study using a qualitative research interview analyzed thematically. Conducted in Depok, West Java, the study involved in-depth semi-structured interviews with 18 participants, encompassing patients from first-level health facilities (FLHF), general practitioners at FLHF, specialist doctors, and management of referral hospital (RH) officers, and staff members of the JKN. The data were transcribed and analyzed using a thematic approach. The study revealed substantial underutilization of respecting patient autonomy within medical contexts under the JKN. Five themes emerged: challenges in the referral system, knowledge and information dissemination, decision-making and autonomy, quality of healthcare services, and systemic constraints and impact. These themes highlight the lack of patient awareness, restricted medical choices, the dominant role of paternalism (a system in which the government or a person in a position of authority makes decisions for other people) in healthcare decisions, and improper informed consent process. The findings suggest that the principles of beneficence and paternalism often overshadow respect for patient autonomy in the JKN system. This raises concerns about the ethical aspect of patient treatment, particularly the need for greater focus on patient autonomy and shared decision-making to align more closely with global medical ethics practices. This study contributes to understanding autonomy in national health insurance systems in developing countries. It highlights the need for systemic reforms to enhance healthcare efficiency and effectiveness while respecting patient autonomy.
Consent: The practice of the Nigerian Orthodontist
Consent: The practice of the Nigerian Orthodontist
Sylvia Etim, Onyinye Dorothy Ume
International Dental Journal, October 2024
Open Access
Abstract
Aim or Purpose
The aim of the study was to survey the knowledge and practices of Nigerian Orthodontists regarding the obtainment of consent before administering procedures capable of modifying the facial profiles of patients.
Materials and Method
This was a 6-months cross-sectional study design involving Orthodontic practitioners in Nigeria. A 14-item questionnaire was administered to participants via google form, consisting of 2 sections. Section A elicited information on socio-demographic data, professional status, and institution of practice. Section B elicited information on the knowledge and practice of consent taking before Orthodontic procedures. Data collected was analyzed using both descriptive and inferential statistics with significance set at P value > 0.05. Ethical approval was duly obtained from the Research and Ethics committee of University of Port Harcourt Teaching Hospital.
Results
There were 66 participants (Male-46; Female-20) with mean age 43.7 +/- 9.26 years. Those who had knowledge of informed consent (64, 97%), verbal consent (57, 86.4%), and implied consent (49, 74.2%), but in terms of practices, most obtained informed (52, 78.8%), next was expressed consent (27,40.9%) and least was surrogate consent (6,9.1%). Informed consent was obtained more for fixed appliance therapy and aligners (62, 94% ) than removable appliances (49,74%).
Conclusion
Most Nigerian Orthodontic practitioners are aware of the importance of obtaining consent from their patients and they do obtain appropriate consent before carrying out Orthodontic procedures.
Enhancing Professional Awareness of Informed Consent : Safeguarding the Rights of Patients and Practitioners
Enhancing Professional Awareness of Informed Consent : Safeguarding the Rights of Patients and Practitioners
Min Ji Kim
Journal of Korean Neurosurgical Society, 30 September 2024
Abstract
Informed consent is a crucial communication process between doctors and patients for obtaining patients’ approval before initiating medical treatment. It is derived from the legal principles of medical contracts and requires doctors to explain the treatment process to patients. Surgeons should be aware of informed consent not only to avoid unnecessary litigation risks but also to provide patients with the right to self-determination. The aim of the study is to help surgeons in Korea understand the legal doctrine on informed consent for practical application. This article reviews the legal doctrine of IC according to 4W1H-why, who, what, when, and how-with judicial cases to communicate effectively with patients in clinical settings. Regardless of seniority or rank, doctors may provide competent patients with information to protect their rights to self-determination. Informed consent should be advanced for patients to consider, discuss with significant others, and determine whether or not to undergo medical treatment. At that stage, patients need to be informed of the necessity, risks, and so on. The most common method of informed consent is an oral explanation utilizing certain forms for documentation. However, the informed consent of patients can be exempted on certain occasions. Optimal informed consent, when implemented, leads to patient-centered care, which significantly improves patient satisfaction and outcomes. Ultimately, it not only protects doctors from litigation risks but also upholds patients’ autonomy.
Researchers experience and views on participants’ comprehension of informed consent in clinical trials in Malawi: a descriptive qualitative study
Researchers experience and views on participants’ comprehension of informed consent in clinical trials in Malawi: a descriptive qualitative study
Research
Dorothy Maxwell Kazembe, Yimtubezinash Woldeamanuel, Solomon Mequanente Abay
BMC Medical Ethics, 27 September 2024
Open access
Abstract
Background
Informed consent is the cornerstone of research ethics. One of its goals is that participants enter research with an understanding of what their participation entails. This paper is a study on how researchers understand the informed consent process. Previous studies have looked at this topic from a research participant perspective. However, few studies focus on the perspectives of the researchers. Therefore, this is an important paper that highlights an important issue (informed consent) from the perspective of those who administer it during research.
Methods
In-depth interviews were conducted with 18 researchers from 3 different research centers in Malawi working in clinical trials. The data was analyzed using open code utilizing the thematic approach to qualitative data.
Results
This study identified that researchers have good awareness of the role of informed consent, how important it is for participants to understand the given information and ways to adjust their practice accordingly when obtaining it in order to enhance participant understanding. According to the research staff, most participants do not really understand all the concepts of the study at the initial visit, they gain more understanding during subsequent visits. It was emphasized that the best method of facilitating informed consent is reading the informed consent to the participant, thus a face-to-face conversation. Long and complex informed consent was identified as one of the barriers to participant understanding of the informed consent. Shortening the informed consent form and having additional conversation with the participants was suggested as one way of improving participant comprehension.
Conclusion
Most of the participants understand much of the information during subsequent visits as you keep reminding them since informed consent is an ongoing process. Existing relationship or trust between a participant and a researcher, may influence participants’ decision and misguide their understanding on the purpose of the study. Adequate time should be allocated to informed consent discussions. Shortening the informed consent forms and having additional conversations with potential participants may help improve their understanding.
Comparison of informed consent for breast cancer surgery in the UK and the Czech republic and patients’ satisfaction with the process
Comparison of informed consent for breast cancer surgery in the UK and the Czech republic and patients’ satisfaction with the process
Monika Rezacova
BMJ Surgery, Interventions, & Health Technologies, 27 September 2024
Abstract
Background
Informed consent is a concept accepted largely in the world, however its interpretation varies. Understanding the diagnosis and process of treatment should be a crucial part of doctor-patient relationship.
Methods
We have assessed 100 patients with a new breast cancer diagnosis (50 in each centre). We have compared the consent forms, risks mentioned to the patient and proposed surgery. A questionnaire was given to patients following the consent process to assess patients‘ satisfaction with information given and possibility of outcome change.
Results
In the UK, patients were given a surgical management plan with multiple potential risks listed on consent. Patients in Czech were given all possible surgical options without specific plan and only few complications. Patients in the UK were satisfied although some of them would appreciate fewer information on risks. Patients in Czech had trust in the doctor’s decision however majority of them would appreciate the exact procedure proposed and more information regarding risks.
Conclusion
Although patients had very different experiences, the vast majority would like to hear the exact type of procedure that is being done and list of significant risks.
Practices of Informed Written Consent for Elective Urological Procedures at a Tertiary Care Hospital in Sudan
Practices of Informed Written Consent for Elective Urological Procedures at a Tertiary Care Hospital in Sudan
Mohammed Elsiddig, Mohammed Hassan
Cureus, 26 September 2024
Abstract
Objective
This study aimed to assess informed consent practices in elective urological surgeries at a tertiary care facility.
Materials and methods
A retrospective cross-sectional survey was carried out between March 1, 2023 and April 1, 2023, at the Department of Urology, Omdurman Military Hospital, Sudan. We included all patients who had undergone elective urological procedures under local, spinal, or general anesthesia. The medical records were accessed to analyze the consent forms’ standards. A total of 42 consent forms were included and analyzed. We use the General Medical Council’s (GMC) Guidance on Professional Standards and Ethics for Doctors: Decision Making and Consent, and the Royal College of Surgeons (RCS) of England’s Consent: Supported Decision-Making as the standard for our study. The GMC and the RCS of England have provided comprehensive and standardized guidelines for obtaining informed written consent, including indications, benefits, risks involved, and alternatives in addition to demographics, patient details, responsible consultant, diagnosis, and title of the surgery, intended benefits, probable risks, type of anesthesia, consenting doctor’s name, designation, and signature, and the patient’s signature and name.
Results
A total of 42 consent forms were included. The diagnosis and the intended surgical procedure were mentioned in all consents. The potential benefits and risks were discussed in 36 (85.7%) and 18 (42.9%) cases, respectively. The type of anesthesia was discussed in 39 (92.9%) of cases. The likely result of not having the procedure and the alternative treatment: Recorded completion rates of 10 (23.8%) and 12 (28.6%), respectively. Patient demographics were completely documented in 41 (97.6%) forms. Senior doctors were only involved in 14 (33.3%) of the consents. Details of the consenting doctor, including name, title, and signature, were present in 30 cases (71.4%), and the date of signing the consent was documented in 38 cases (90.5%). The completeness of the consent form correlated with the level of the doctor obtaining it, with consultants achieving the highest completion rates (100%), followed by registrars (66.7%) and medical officers (35.7%).
Conclusion
The current practices of informed consent were found to be substandard. Handwritten consent forms do not adhere to the recommended guidelines for informed consent in elective urological procedures. It is preferable to utilize a pre-designed consent form, allowing for personalized additions based on the patient’s specifics. Our recommendation is to organize an educational session for junior doctors to emphasize proper consent procedures, and deepen their knowledge of common urological elective procedures, and associated risks. This approach promotes adherence to best clinical practices and minimizes the risk of legal challenges.
Application of Standard Informed Consent Procedure Amongst Practicing Anesthetists in Tertiary Care Hospitals of Karachi
Application of Standard Informed Consent Procedure Amongst Practicing Anesthetists in Tertiary Care Hospitals of Karachi
Asif Hassan, Mahendar Wanwari, Adeel ur Rehman, Tarique Aziz, Kashif Naeem, Fahad
Journal of Health and Rehabilitation Research, 4 August 2024
Abstract
Background
Informed consent is a critical component of anesthesia practice, ensuring patient autonomy and safety. However, variability in the application of consent procedures among anesthetists may impact patient understanding and care quality.
Objective
To evaluate the application of standard informed consent procedures among practicing anesthetists in tertiary care hospitals in Karachi.
Methods
A cross-sectional study was conducted from February 15, 2021, to August 14, 2021, across five tertiary care hospitals in Karachi. A total of 112 anesthetists, including consultants and residents with at least two years of experience, were recruited through consecutive sampling. Data were collected using a custom-made 16-item questionnaire. Responses were scored from 0 to 64, with scores ≥32 considered acceptable. Data were analyzed using SPSS version 25, employing descriptive statistics and Chi-square tests for comparisons.
Results
The mean age of participants was 34.04 ± 8.15 years, with 5.43 ± 5.9 years of experience. Compliance with consent standards was 99.11%, with 111 out of 112 participants scoring ≥32. No significant differences were observed across age, gender, or qualification (p > 0.05).
Conclusion
Anesthetists in Karachi showed high adherence to informed consent standards, though enhancements in risk disclosure are recommended to further improve patient care.